Diverticulosis
Here we will explain what diverticulosis is, why people get it and how to treat it. This is a highly variable disease, and our view is that each patient requires a personalised approach to treatment. If you have any questions or you would like a consultation, please get in touch here.
What is diverticulosis?
Diverticulosis is a common condition of the colon that causes small pockets to form along its length. These are caused when the innermost lining of the bowel (called the mucosa) is forced out by pressure from within the lumen of the bowel (figure 1). It is now generally thought that these are caused by chronic low grade inflammation in the gut that leads to weaknesses forming in the bowel wall, typically where blood vessels (known as the vasa recta) pass through the bowel wall.
Diverticulosis with the small pockets visible along the colonic wall
Figure 1.
Diverticulosis is a western disease, and it is very common; it affects 50% of people over the age of 60, and it leads to 2.7 million outpatient appointments and 300 000 hospital admissions in the USA each year. It is becoming more common, and there has been a 21% rise since 2003. The prevalence in younger patients is also increasing.
What symptoms does diverticulosis cause?
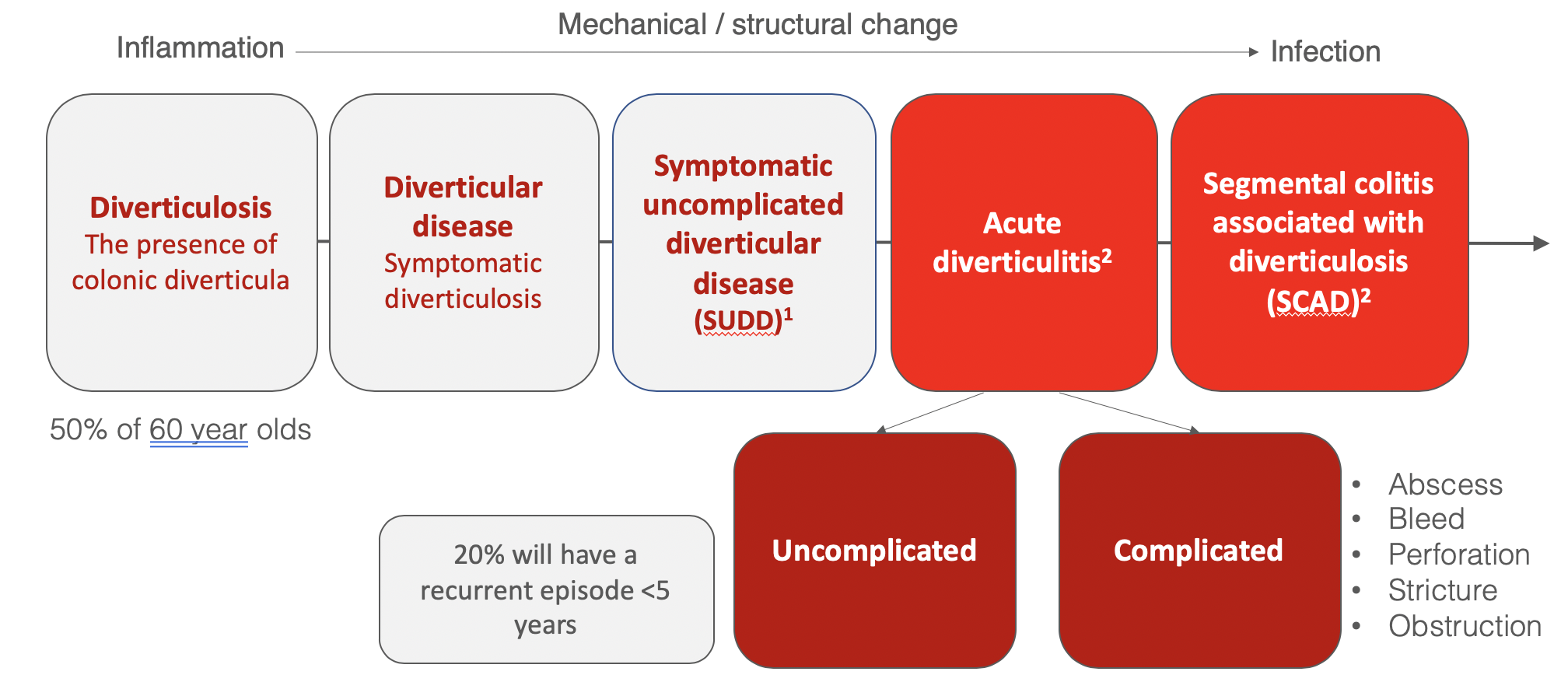
Most people with diverticulosis are asymptomatic and probably never know they have the condition. It is commonly found during routine colonoscopy or CT scans. However, it represents a spectrum of disease (figure 2) and this is because diverticulosis is now thought to be an inflammatory condition of the gut. Some people may have diverticulosis and be very symptomatic. These symptoms may include bloating, constipation, abdominal pain and it presents much like Irritable bowel syndrome. This is known as Symptomatic Uncomplicated Diverticulosis (SUDD).
A map of the different types of diverticular disease
Figure 2
Why do people get diverticulosis?
Patients suffer from this condition because of a combination of lifestyle factors and their genetic predisposition (figure 3). The most important modifiable risk factors are largely dietary and the most important of these is thought to be a low fibre diet. The chance of getting diverticular disease reduces with every 5 g/day fibre you take, but this reduction does depend on the type of fibre you eat. Red meat intake and processed meat is associated with an increased risk of diverticulitis (and bowel cancer). Substitution of poultry or fish for one serving of unprocessed red meat per day can reduce your risk. It is also associated with Vitamin D levels, and low levels of vitamin D are associated with an increased risk of diverticulitis. Smokers and those that have had gall stones are also at an increased risk. However, it is also very likely that that the many trillions of bacteria, yeasts, viruses and parasites that in habit the gut (know as the microbiome) also play an important role. However, this work is only just emerging.
Causes of diverticulosis
Figure 3
What should I do if I have uncomplicated diverticulosis?
It is important that you recognise that this suggests your diet may not be doing your bowel any good and that you need to change some of your lifestyle factors to improve your health and prevent this becoming worse. This means you need to do the following:
1. Aim to eat at least 30g of fibre / day. Information on how to do this can be found here
2. However, make changes to your diet slowly, and increase the fibre by 5g each day over a week until you reach the recommended daily intake or you will be bloated.
3. You need to do this for life! A healthy gut requires a fundamental change in many peoples dietary behaviour.
4. Reduce the amount of red meat and processed meat you eat. Try replacing one meal a day with white meat (poultry or chicken).
5. You CAN EAT NUTS and seeds! It is a common misconception that people with diverticulosis should not do this as they can lodge in the pockets of mucosa. However there is no evidence this is bad for you.
6. Stop smoking – if you do! (And that doesn’t mean start vaping as the consequences of this on the bowel are not known)
7. Exercise regularly.
8. Ask your GP to check your Vitamin D levels.
9. Avoid taking Ibuprofen or drugs known as NSAIDs unnecessarily.
10. Try taking a bulk forming laxative like methylcellulose if you are constipated. Your GP can help prescribe it.
11. Drink enough water – you need about 2 litres of fluid a day and it’s important for maintaining soft bowel motions.
12. Loose weight – if you do all the above, this will happen anyway!
Have you noticed this is the same advice for reducing your risk of cancer or heart disease? This is no accident and its because the same biological processes that cause diverticulosis also cause these diseases.
How do you treat SUDD?
This a more difficult and it requires a more personalised approach. All of the advice above is important, but sometimes other approaches are also needed.
This is because some evidence suggests patients with SUDD have bowel which is overly sensitive to stretch which causes pain. They also have levels of inflammation that are higher than in other more mild forms of diverticulosis.
The trial data for the use of anti-inflammatory medicines like Mesalazine has been disappointing, and they are not typically recommended. Drug trials with specific antibiotics such as Rifaxamin have also not shown an effect.
I do recommend that patients try the FODMAP diet and information can be found here on this here
However, patients should see a gastroenterologist or surgeons with a specialist interest in this condition. I favor the creation of a personalized diet and even though the evidence for probiotics is limited, and I do selectively recommend the probiotic therapies below.
So, what is diverticulitis?
Diverticulitis describes acute inflammation of a segment of colon with diverticulae. It does not mean that there is infection, but that the bowel is inflamed. Sometimes, a diverticulum is obstructed with a hard lump of faeces, known as a freckling, and it its though that this obstructs the diverticulum and drives the infection (figure 1). At surgery the bowel appears looks thickened, stiff and oedematous. Patients will often complain of pain in the left side of the abdomen, and develop a temperature and an altered bowel habit.
The severity of diverticulitis ranges, but it is often described in terms of being ‘uncomplicated’ or ‘complicated’ (figure 2). Uncomplicated means it can be treated with simple medicines and life style advice, while complicated means that the diverticulitis has caused a structural change in the bowel (like a perforation, stricture or obstruction). Occasionally, a diverticulum can be obstructed by faeces and this can lead to perforation and the development of an abscess. This can make patients very unwell indeed and it may require treatment in a hospital and occasionally it needs surgery.
If you have severe abdominal pain, a temperature or fever or if you are concerned please seek help from your doctor.
How do you treat diverticulitis?
The first step is to rule out other diagnoses and to make sure there is no complication of the diverticulitis. So, if you suspect you may have this, you need to see a doctor. In this situation, I will typically perform a blood test and perform a CT scan. A blood test called a 'CRP' is particularly good at predicting the severity of the disease. These tests allows the doctor to rule out other diagnoses and target the treatment.
Treatment really depends on the severity of the disease:
1. Mild disease
Evidence now suggests this can be managed safely at home. The most controversy at the moment concerns the use of antibiotics. 8 randomised control trials have now been performed and the consensus is that in mild disease antibiotics DO NOT make diverticulitis better. Many Doctors will prescribe antibiotics for this condition but it is likely not to help.
Take regular pain killers but avoid ibuprofen. Take a small dose of stool softener if you are constipated and plenty of fluids.
Rest the gut. This means a fluid or liquid diet only while you have severe pain and your gut is not working properly. Avoid a high protein diet, rich food, spicy food and alcohol.
Patience – you are going to feel unwell for about 5 to 10 days, and you need to take time off work and rest.
The prognosis is good. In patients managed this way, less than 5% will need surgery. However, about 20% of patients with diverticulitis will have recurrent episode within 5 years.
2. Moderate or severe disease
This requires specialist input and your GP needs to refer you urgently to a colorectal surgeon for management. If you would like to be seen by a specialist click here
Treatment depends on the presence of infection, its severity and the presence of other possible complications from diverticulitis. This is usually determined from a CT scan.
In the presence of a localized abscess, it may be possible to treat this with antibiotics. However, sometimes it is necessary to perform a CT guided drainage. Surgery is only performed when patients are severely unwell, and there is significant contamination of the abdomen with pus or faeces. This requires an emergency operation and three procedures are commonly performed:
Surgery for diverticulitis
a. A laparotomy (a big cut on the tummy) removal of the diseased segment with the perforation and the formation of a colostomy (a bag). Many patients are worried about the presence of a bag, however this is a life saving treatment and it is usually reversible.
b. A laparoscopy (a key hole operation) with drainage of the infection and the insertion of drains. The benefit is that the patient avoids a colostomy, although this is put in about 14% of patients managed this way. When the patient is recovered, they can have an elective operation to remove this segment of disease and the bowel is rejoined with lower rates of colostomy formation. But, a recent study found that patients that underwent this procedure have three times the risk of developing peritonitis or requiring emergency surgery. The hospital stay can be long and the drains may need to remain in for several weeks.
c. Laparoscopic (key hole) removal of the diverticulitis segment with a primary anastomosis (join) with or without a temporary ileostomy. The benefit of this, is that the stoma is more likely to be reversed as this is a much simpler operation. It also means that the patients is definitively treated at one operation. However, this is a high risk join to make, and this approach needs to be used in a highly selective way.
Sometimes, surgery is performed when the patient has recovered from their initial surgery or for the treatment of complications. This is a highly specialized type of surgery and should only be performed by a specialist colorectal surgeon.
I advocate laparoscopic surgery although the conversion rates of laparoscopic sigmoidectomy for complicated with diverticulitis are double that for cancer and as high as 30%.
I also advocate for the temporary stenting of the ureters (these drain urine from the kidney to the bladder) to protect them during surgery as these are commonly injured. 36% of all ureteric injuries occur in this condition.
Surgery is not without its risks. Elective surgery has a 10% anastomotic leak rate, and there is a risk of incontinence; 25% of patients complain of an altered bowel habit, abdominal distension or cramping. The rate of diverticulitis recurrence after resection (5-11%) is similar to the rate of recurrent hospitalized events (4-13%) if no surgery and the risk of recurrence is higher in young patients, smokers and in women.
The American Gastroenterology Association suggests against elective colonic resection in patients with an initial episode of acute uncomplicated diverticulitis. My view is that the the decision for surgery is highly personalised and should be made on an individual basis.
Surgical treatment for acute diverticulitis
How do I stop diverticulitis happening again?
This another tough question as the evidence to support interventions is very limited. However, I would advocate all of the advice given for the treatment of diverticulosis. This is about making a concerted attempt to reduce the amount of inflammation in the gut and to improve gut health.
I work with my dietician and gastroenterology colleagues to create a personalized plan for patients based on the best available evidence.
Should I have a colonoscopy after an episode of diverticulitis?
This is a surprisingly controversial question. In one large scale retrospective study performed in Scandinavia, those who had no colonoscopy, had nearly three times the risk of colon cancer compared with those without both diverticulitis and colonoscopy. The risk of having a cancer hidden in a segment of colon affected by diverticulitis is around 15/1000 cases.
Colonoscopy is not without its risk, and it can be complicated in frail patients with severe disease. This is because there is a risk of perforation or making a hole in the colon.
The American Gastroenterology Association states the current evidence base for this diagnostic test is low.
My view is to make a decision on individual patient basis. This is based on an individuals specific risk, the presentation of the condition and their risk profile for colonoscopy and the associated bowel preparation.
Patient information and links
There is a lot more we haven't discussed. If you want to find out more, I recommend the links below:
CORE charity: http://corecharity.org.uk/gut-liver-and-pancreas/gut/diverticular-disease/
NHS Choices: https://www.nhs.uk/conditions/diverticular-disease-and-diverticulitis/
The association of UK dieticians: https://www.bda.uk.com/foodfacts/fibrefoodfactsheet.pdf
Evidence and guidelines
More evidence to support the recommendations made in this blog can be found below:
NICE https://cks.nice.org.uk/diverticular-disease
WSES: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4966807/
Colorectal surgeon consensus: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5714804/
ACPGBI position statement: https://www.acpgbi.org.uk/content/uploads/Position_Statement_Elective_Resection_for_Diverticulis.pdf
Fibre: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4145436/
Probiotics: https://www.ncbi.nlm.nih.gov/pubmed/27014757
Meat Consumption: https://www.ncbi.nlm.nih.gov/pubmed/28069830
Antibiotics in diverticulitis: https://onlinelibrary.wiley.com/doi/abs/10.1111/codi.14013